The importance of Clinical Technology and vital medical equipment
August 4, 2016 | By Toni Calliva
Clinical technologists are technologically sophisticated staff members who are intimately involved in many aspects of healthcare, they are instrumental in bridging the gap between clinicians and engineers. They don’t work directly with patients, but with the technology used to support patient care. Clinical Technologists are capable of applying their knowledge to assist in the diagnosis, treatment and rehabilitation of patients.
We recently had a chance to speak with Earl Isaacs, Head Clinical Technologist at the Red Cross War Memorial Children’s Hospital (RCWMCH) in Cape Town, South Africa as well as Hans Human, Former Head of Clinical Technology (1999 – 2011) at the RCWMCH. Hans Human retired in 2011 but continues to be a big supporter of the hospital.
Human gave us an overview of the roles and responsibilities of a Clinical Technologist at the RCWMCH, he explained that a Clinical Technologist registered with the South African Health Professionals Council as a graduate in Critical Care is able to use biomedical equipment to perform diagnostic, therapeutic and organ support on patients in Anaesthetic departments, theatres, Intensive Care, Trauma and high care areas. Tasks performed include the stripping and cleaning of specialised equipment after use, the set up and calibration of clean equipment before use; using the equipment to perform procedures or assisting medical specialists or other health professionals who perform procedures on patients. The procedures performed on patients include invasive and non-invasive vital signs monitoring, ventilation and oxygenation, blood tests, control of body temperature, resuscitation, and transport of ventilated patients for specialised procedures outside the intensive or high care area. Administrative tasks include stock control of equipment and re-usable and disposable items. Senior Clinical Technologists are responsible for in-service training of clinical technology students and all other health professionals in the use of the equipment in their area.
HOW IT STARTED
Earl Isaacs started at RCWMCH in the 90’s as a junior “before there even was an actual clinical technology department in place or a dedicated role for a technologist”, Isaacs now oversees three clinical technologist posts, one to cover theatre and two for the ICU.
Isaacs was working with Hans Human, Head of the Clinical Technology department at the Groote Schuur hospital when Prof. Andrew Argent, Head of ICU at the RCWMCH, contacted them. “Prof. Argent requested that someone from our department come to the Red Cross Children’s Hospital to “gooi a oogie” or as one would say in english – “cast an eye” over the workings in their ICU department” says Isaacs.
Their team would do monthly visits to the RCWMCH and slowly, over time they worked on getting an in-house Clinical Technology service up and running.
“We started the clinical technology service at RCWMCH in 1999 when children were cared for in four ICU’s. Two medical and two surgical ICU’s separated for paediatric and neonatal patients. At the time the development of one ICU for all categories of patients run by Intensive specialist doctors was well underway. The nursing service was provided by specialised nurses for each separate unit. The equipment used in each ICU area differed depending on the needs of the unit. Most of the equipment in use did not represent the latest technology.” describes Human.
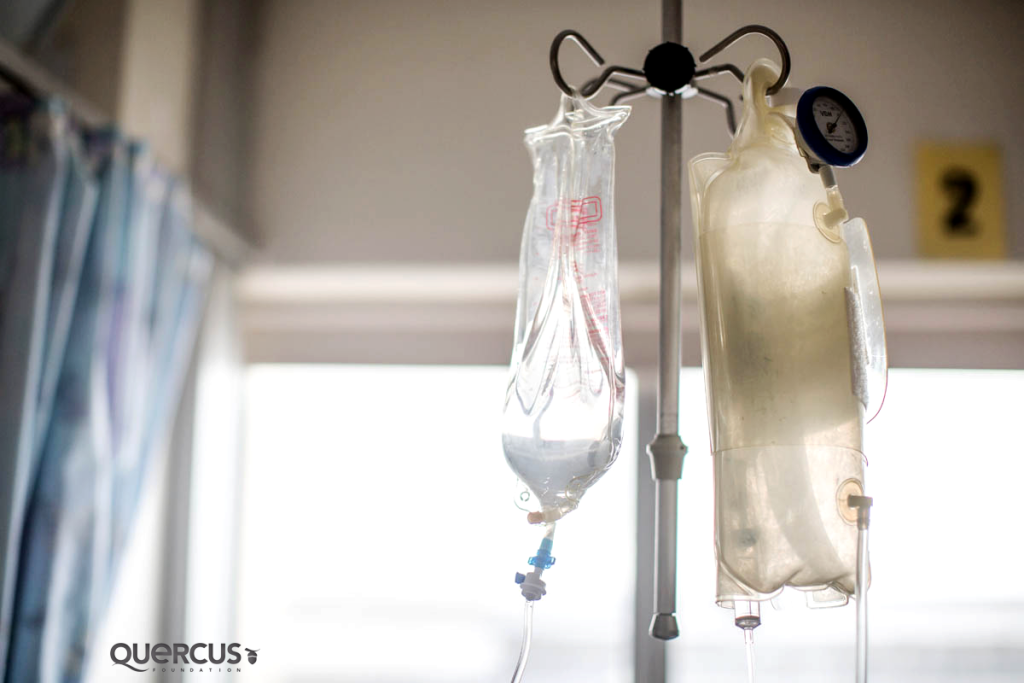
TAKING A LOOK AT VITAL EQUIPMENT
Isaacs tells us about 3 pieces of medical equipment that play a vital role in supporting critically ill children at the RCWMCH and how maintaining them is a very important part of what they do.
Monitors:
“Monitoring vital signs is important. The monitors that we have in ICU are, obviously, the best monitors you can have. They can monitor heart rate; ECG; invasive blood pressure; non-invasive blood; temperature and various other things. Making sure that monitors work correctly is an important part of what we do.
It is challenging if the nurse comes to me and says, “The monitors not working, what do I do?” because I don’t have a spare monitor that can do the same things as the other one.
Ideally, every monitor should be working. If one goes down, we should have two spare, so that we can put a replacement one up immediately. We should always have more equipment than patients incase anything should break, we would have two or three spare.
We also need a proper monitoring system in the future so we can go paperless! That’s really where we want to go. We would then be able to pull up all the patient’s lab data and chemistry results on one screen. Not only save the medical staff a lot of time but it would also reduce the chance of cross infection caused by staff moving between departments.”

“Ventilators or ‘breathing machines’ are extremely important pieces of equipment supporting children in critical care. Maintaining them is a very important part of our job.” -Earl Issacs, Head of Clinical Technology Department, Red Cross War Memorial Children’s Hospital, SA. Photo Credit: Karin Schermbrucker, Slingshot Media, SA
Ventilators:
“Breathing machines or ‘ventilators’ are extremely important pieces of equipment supporting children in critical care. We deal with intervention basic to nasal pump oxygen, the CPAP machine-which is the high flow, air lows and then the Newport ventilators for the Servo I machines, which are the breathing machines. Maintaining these is a very important part of our job.”
The challenge is “we never have enough Servo I ventilators, because that’s the best ventilators we use. So at the moment we’ve got 22 patients, but we’ve only got 13 Servo I ventilators. Once those are all in use, the other patients needing incubation, then need to go onto a Newport E100M, which is a much more basic ventilator. It’s aimed more towards your trauma cases of patients needing short term ventilation in a medical emergency setting. The Servo I, on the other hand, is a very specific machine for lung problems, lung pathology. It’s a really nice machine, because people can fiddle with it more, they can see more like waveforms, pressure, flow, time, and those kinds of things. The moment you can adjust more, the doctors feel more comfortable, because they can see where the gas is and where it’s flowing to. What they would really like to have is one Servo I per patient per bed that needs ventilation.”
Infusion devices:
“Then, we have infusion devices, which is equipment that dispenses medication. Some need to be given very accurately and they go into, what is called, a syringe driver, which basically mixes the drug and puts in a 50ml syringe so you can measure it down to the second decimal point. This is integral in terms of accuracy and can be used for medication such as adrenaline, dobutamine and dopamine.”
[Does it have to be that precise, because you are dealing with such small patients?]
“Yes, those drugs are worked out in micrograms per kilogram per minute. These dosages are supposed to be measured according to weight and the condition of the patient.”
WORKSHOP AND STORAGE SPACE
Another challenge that the department faces is the lack of workshop and storage space for it’s Clinical Technologists. The current upgrade and expansion project at the RCWMCH will provide:
A workshop for Clinical Technologists to test and repair their equipment
Office facilities for clinical and research staff
Safe and adequate storage space for high value equipment.
“At the moment we actually have to use two patients’ bed spaces to check the machines and park them on standby, we use bed space ’12’ and ’13’ inside the ICU to store the ventilators and the equipment that medical staff need in a hurry, like: nitric oxide, CPAPs, Airvo and ventilators.The most important thing is storage space for equipment. I don’t think people realise how difficult it is to find storage space for the ICU’s equipment, we get whole cages full of equipment from neurosurgery, equipment that measures brain saturation, brain oxygenation, intracranial pressure, plus cardiology equipment. Space wise, those are big issues.” explains Isaacs.
“We are currently all squashed into a small space between bed 12 and 13, which is in the corner of the ICU, so that we can check machines and deal with consumables. It’s quite inconvenient, because it means that the technologists and the clerk who packs up all the stock, and the housekeeper – we all share the same space. It’s just one big rectangle. When our stores deliver their supplies, it’s becomes a big issue about where we’re going to put them, especially with the bulk equipment. All the while taking up precious bed space for sick patients.”
Quercus Foundation has partnered with the Children’s Hospital Trust (CHT), the South African registered charity that raises money on behalf of the Red Cross War Memorial Children’s Hospital and are currently trying to raise funds to support the upgrade and expansion of the ICU as well as to purchase new vital equipment needed to support critically ill children. You can help too by donating, your support will make a big difference to little lives.