Breatheasy report 2015 – 2016
April 13, 2016 | By Toni Calliva
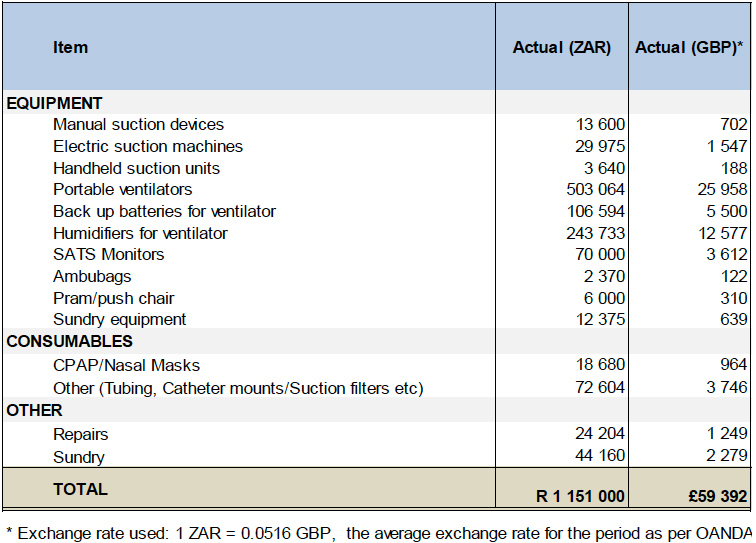
We are pleased to report that between January and December 2015, we successfully funded the Breatheasy Programme with £59 392 (R1,151, 000).
The Breatheasy Programme is a unique specialist nurse-led initiative at the Red Cross War Memorial Children’s Hospital (RCWMCH) that empowers parents of children reliant on a tracheostomy or artificial ventilation for breathing to provide safe care for their children at home.
Tracheostomy patients around the world characteristically face lengthy hospital stays. Through careful training and support of families, the Breatheasy programme ensures that children with tracheostomies instead return home to their families and communities, as soon as they are medically stable.
Once home, they are monitored as outpatients by the programme, while family members take responsibility for routine day-to-day medical care (such as changing and suctioning the tracheostomy tubes). Breatheasy’s training enables families to provide home care equivalent to that of a professional nurse in the tertiary health sector.
The equipment necessary for home-care is provided by the Breatheasy programme to families: this includes suction machines, humidifiers, ventilators, among others, as well as a range of associated consumables required for safe care.
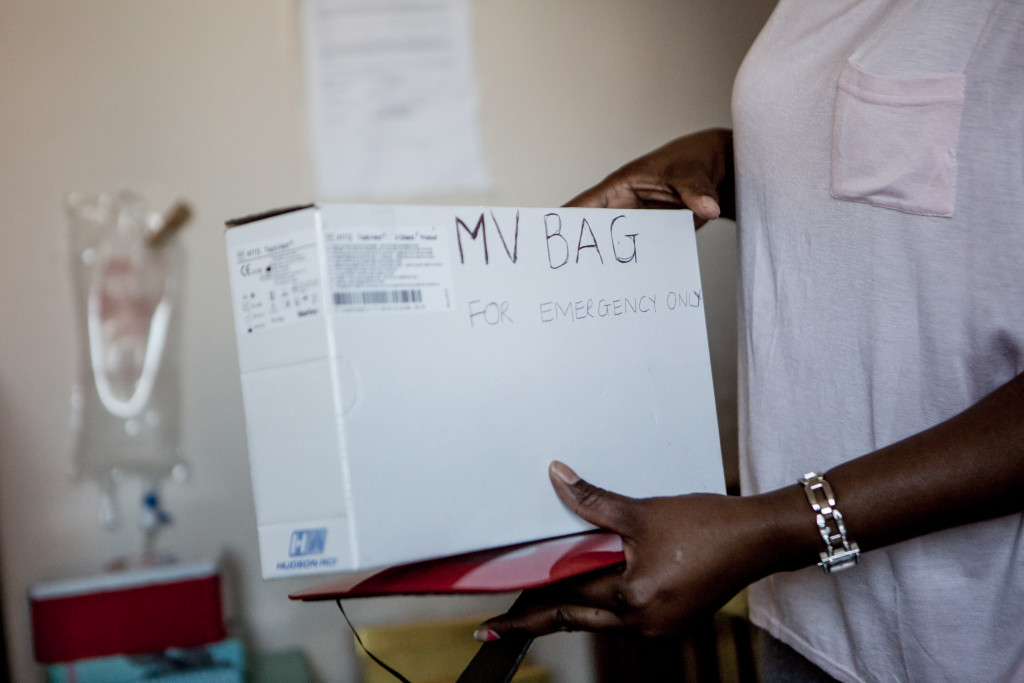
Breatheasy equipment set up and in use at a patients home. The equipment necessary for home-care is provided by the Breatheasy programme to families: this includes suction machines, humidifiers, ventilators, among others, as well as a range of associated consumables required for safe care.
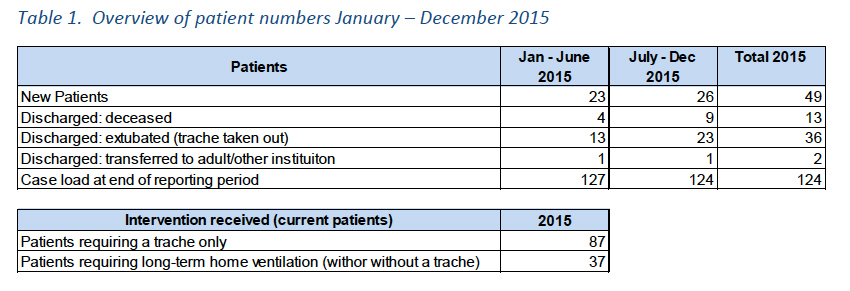
OVERVIEW OF PROGRAMME, JANUARY – DECEMBER 2015
- BENEFICIARIES
Between January and December 2015, 49 children entered into the Breatheasy programme. Fifty-one children were discharged from the programme over the period, the majority due to their recovery and extubation – the removal of their tracheostomies once no longer required for breathing. In addition, 13 children died, and two transitioned to adult care, leaving 124 children on the programme case load at the end of December.
For as long as they remain clinically stable, these children continue to be followed up as outpatients. Almost one-third of children currently managed on the programme require either 24 hour or nocturnal ventilation: this is a higher proportion than has generally been the case in the past. It is likely that as diagnoses improve, the numbers of ventilated children in the programme will continue to increase.
Far greater numbers of children have in addition benefited indirectly from the programme, thanks to the availability of beds at Red Cross Children’s Hospital that would otherwise have been occupied long term by children with tracheostomies and on ventilation.

Diego Biasi, with a patient and his mother in the Breatheasy Ward at the Red Cross Children’s Hospital, SA, 2015.
- PARENT / CAREGIVER TRAINING
Once a tracheostomy (opening in the airway) has been surgically created in the airway of a child, a trachea tube is inserted to keep the opening and airway open. The trachea tube has to be suctioned regularly and as well as taken out, cleaned and replaced daily. Children on ventilators are considered to be ‘high risk’ and require additional day-to-day medical care at home.
Parents or alternative primary caregivers of every child who entered the Breatheasy programme during the reporting period were trained by Sr. Jane Booth and the Breatheasy team to perform these critical functions for their children. In instances without clinical complications, parents/caregivers spent approximately four weeks in the ward at Red Cross Children’s Hospital, during which time they received the necessary training for home care.
This included:
- Training on the equipment
- Supplies and medication needed
- How to clean the equipment
- How to change and clean the tracheostomy
- How to suction, how to feed, bath and transport children with tracheostomies or on ventilation as well as how to support their speech development, and what to do in an emergency.
- The programme was individualised to every child and family for his or her unique condition, home environment and needs.
In addition, the Breatheasy team facilitates daily group sessions, which provide mothers and other caregivers with a forum to obtain further information and practical skills, as well as to discuss any issues important to them. This group provided the space for the caregivers to support each other and many remain in contact once their children have been discharged.
Upon discharge, all families were provided with a detailed and graphic instruction manual as well as all the necessary equipment and supplies needed for home care.

Program benefits: Countless mothers and other caregivers are empowered, through the affirmation of their ability to manage their children’s needs.
- BENEFITS OF THE PROGRAMME
The Breatheasy programme’s focus on getting children back home as quickly as possible has numerous positive benefits for children and their families:
- Children’s development and quality of life is improved as they are able to grow up within their families and are integrated into their communities. The well-documented adverse effects of long-term hospitalisation, such as emotional deprivation, social isolation, and the risk of hospital acquired infections, are avoided.
- Children’s separation from their mothers is limited. Research emerging from the neurosciences and human biology indicates that the longer infants and children are separated from their mothers, the more their ability to adapt in ordinary life circumstances is affected. The scientific evidence clearly indicates that mother-child interaction is a key determinant of a child’s health outcome.
- The incidence of complications (such as blocked tracheostomy tubes and infection) is lower at home than in hospital. In a developing country such as South Africa, children are eight times more likely to survive under their mother’s care at home, than in hospital.
- Countless mothers and other caregivers are empowered, through the affirmation of their ability to manage their children’s needs.
- The disruption and cost to families of having a child in long-term hospital care is substantially reduced.

Sister Jane Booth discusses the benefits of the Breatheasy programme with Diego Biasi. Breatheasy Ward, Red Cross Children’s Hospital, SA, 2015.
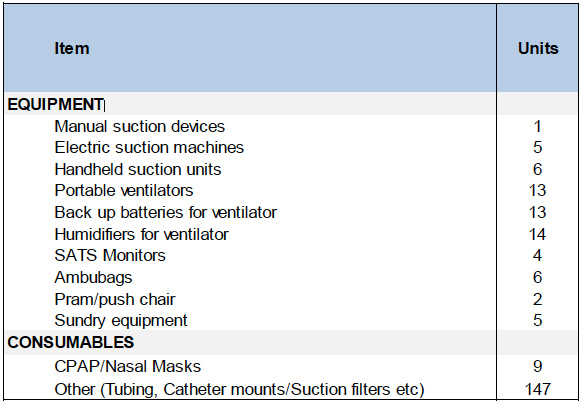
- EQUIPMENT PURCHASED
The Breatheasy programme supplies families with equipment essential for children’s tracheostomy care at home. Wherever appropriate, equipment is returned to the programme once it is no longer needed by children. However there is a consistent need for new equipment for new patients, as the programme continues to grow and when equipment can no longer be repaired or recycled. Equipment generally has a lifespan of approximately 5 years after which it must be replaced. The precise combination of equipment required by the programme each year depends on the specifics of the patients’ conditions that year.
The following table provides an overview of the key items procured by the programme for children’s home care over the reporting period.
FINANCIAL REPORT
Every child who passes through the Breatheasy programme is provided with a manual suction device, either as their primary suctioning equipment or as a backup in the case of electricity failures. In 2015, more than half of the Breatheasy expenditure was related to patients requiring ventilators, a function of an increase in these patients entering the programme during the course of the current cycle.

Training: Medical staff member shows a patients mother how to use the manual ventilation pump, Breatheasy Ward, Red Cross Children’s Hospital, SA, 2015.

Tracheostomy patients around the world characteristically face lengthy hospital stays. Through careful training and support of families, the Breatheasy programme ensures that children with tracheostomies instead return home to their families and communities, as soon as they are medically stable.
OTHER PROGRAMME HIGHLIGHTS, JANUARY – DECEMBER 2015
- The programme has been honoured with two awards this year for its ground-breaking work: In July, Sr. Jane Booth was awarded the Critical Care Society of Southern Africa’s President’s Nursing Award, the highest accolade awarded by the Society, in recognition of her outstanding service to critical care in Southern Africa. In October, the programme was awarded a Special Ministerial Award through the Centre for Public Service Innovation, a national government initiative that operates under the portfolio of the Minister for Public Service and Administration.
- In April, the Breatheasy Programme was profiled on a BBC Series on Innovation in Africa, as one of only two initiatives profiled from South Africa (See http://www.bbc.com/news/health-32162626 to view the insert).
- The programme was also profiled in the official magazine of the provincial Department of Health, in which it was lauded for “breath[ing] the Western Cape Government’s motto of ‘better together’ by proving that healthcare is a collaborative effort that calls for united action by families, communities, local authorities and healthcare workers”.
- In addition to the clinical work of the Breatheasy Programmes, Sr. Jane Booth has participated in various conferences and workshops during the course of the year in order to profile the initiative, and share its approaches. Perhaps most valuably, she presented on paediatric tracheostomy care and home care at the annual South African GP update, attended by GPs from around the country, at a workshop for registrars at Red Cross Hospital, as well as at the international conference ‘Building children’s nursing’ attended by 128 nurses from 12 countries.

Diego Biasi (Founder Quercus Foundation), Chantel Cooper (Children’s Hospital Trust), Doctor and a family in the Breatheasy Ward, Red Cross Children’s Hospital, SA, 2015.
GRATEFUL
It has been such an honour to support Sister Jane Booth, her dedicated team and this amazing initiative that is so profoundly invested in supporting each child’s recovery.
We would also like to thank the dedicated staff at the Children’s Hospital Trust (an organisation who help to raise money on behalf of the RCCH) for presenting us with the opportunity to meet so many beautiful and brave children, their loving parents and for allowing us to share some of their stories.